Keratoconus diagnosis is made by performing a complete eye exam including a slit lamp exam, a topography study which evaluates the curvature as well as the thickness of the cornea. These tests also help monitor progression over time.
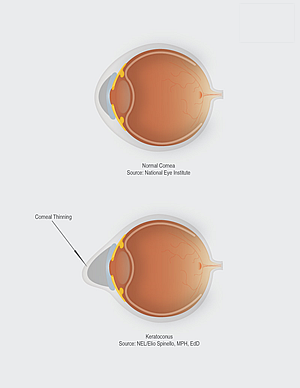
Genetics have a role in keratoconus as well as chronic eye inflammation. Eye rubbing has also been found to contribute to the development of keratoconus.
This office procedure employs a combination of Riboflavin solution and ultraviolet light to create new collagen links that lead to a stiffer cornea. The goal is to strengthen the collagen to prevent further deformation of the cornea and progression of keratoconus.
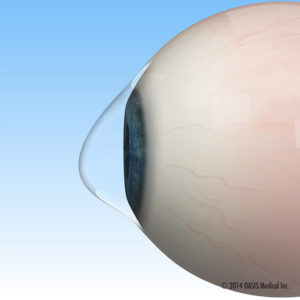
These gas permeable and scleral lenses which have predictable and regular contour are fitted and worn during waking hours to restore vision.
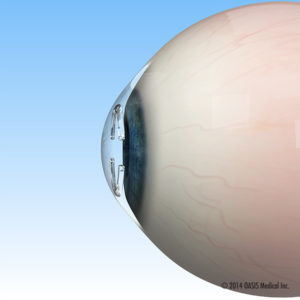
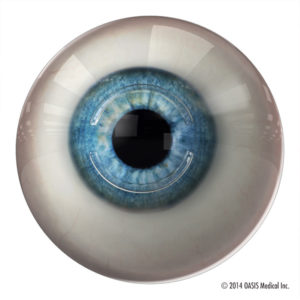
Implantable corneal ring segments are inserted into the middle layer of the cornea with the assistance of femtosecond laser. They are positioned so that they will help flatten the cornea and lessen the astigmatism. This can improve uncorrected vision, but contact lenses may still be required for best corrected vision. Intacts do not prevent progression of keratoconus.

© 2025 Washington Eye Physicians & Surgeons
The material contained on this site is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider.